Background: Mini-hyper-CVD plus inotuzumab ozogamicin (InO) followed by sequential blinatumomab (Blina) is effective in both older adults with newly diagnosed B-cell ALL and in relapsed/refractory disease. We hypothesized that concomitant administration of these agents in a “dose-dense” (DD) fashion would also be safe and effective in B-cell acute lymphoblastic leukemia (ALL), leading to rapid measurable residual disease (MRD) negativity.
Methods: This is a retrospective analysis of patients (pts) with B-cell ALL who received DD mini-hyper-CVD + InO + Blina outside of a clinical trial. All pts received mini-hyper-CVD alternating with mini-methotrexate and cytarabine in combination with InO. To be evaluable for this analysis, Blina must have started prior to day 21 of the first cycle of therapy. Pts were included if they received this regimen for 1.) frontline induction, 2.) treatment of MRD-positive remission, or 3.) salvage therapy for relapsed/refractory (R/R) disease.
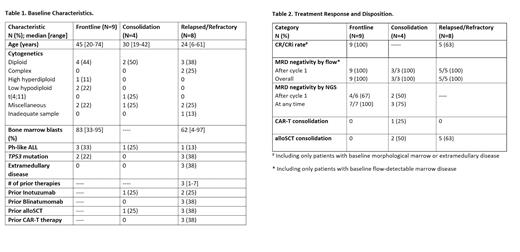
Results: Between 7/2020 and 1/2023, 21 eligible pts were treated (Table 1 ). The median age was 48 years (range, 6-74 years); 3 pts (all in the R/R cohort) were <18 years old. 9 pts (43%) were treated as frontline therapy, 4 (19%) for treatment of MRD (3 for flow-positive MRD and 1 for persistent FISH for t[4;11]), and 8 (38%) for R/R disease. In the MRD cohort, 3 pts were in first CR and 1 was in second CR; 1 pt received prior InO and 1 had prior allogeneic stem cell transplant (alloSCT). In the R/R cohort, pts were heavily pretreated, with a median number of prior therapies of 3 (range, 1-7); 2 pts received prior InO, 3 pts received prior Blina, 3 pts had undergone prior allo SCT, and 3 pts had received prior chimeric antigen receptor T-cell (CAR-T cell) therapy. Three pts (all in the R/R cohort) had extramedullary (EM) disease, 2 outside of the CNS without marrow disease and 1 with CNS disease and bone marrow MRD by flow.
Pts received a median of 2 cycles (range, 1-5) of a dose-dense regimen. All pts received 0.9 mg/m 2 InO in cycle 1, except for 1 pt in the R/R cohort who received 0.6 mg/m 2 due to myelosuppression with prior InO. Themedian cumulative dose of InO was 1.2 mg/m 2 (range, 0.6-2.7 mg/m 2). Blina was started on a median of day 4 (range, day 4-17) of the first cycle of chemotherapy. Blina was started by day 7 in 16 pts (76%).
In the frontline cohort, all pts (100%) achieved CR/CRi (CR in 8 pt and CRi in 1 pt), all after cycle 1 ( Table 2). All pts in the frontline cohort achieved flow MRD negativity. 7 pts were evaluable for bone marrow next generation sequencing (NGS) MRD (sensitivity 10 -6). Of these, 4/6 (67%) achieved NGS MRD negativity after cycle 1, and all 7 evaluable pts (100%) achieved NGS MRD negativity. In the MRD cohort, all 3 flow-positive pts became flow MRD negative after cycle 1; the pt with positive FISH for t(4;11) became FISH-negative after cycle 2. 3 of the 4 pts in the MRD cohort (75%) became NGS MRD negative. Overall, 5 of the 8 pts (63%) in the R/R cohort achieved CR/CRi. Among 5 evaluable pts in the R/R cohort with marrow disease (including the pt with CNS disease and MRD-positive marrow), all achieved flow MRD negativity after cycle 1. Overall, 7 pts (33%) underwent consolidative alloSCT (2 in the MRD cohort and 5 in the R/R cohort), and 1 pt in the MRD cohort underwent consolidative CAR-T cell therapy.
The treatment regimen was well tolerated. No patients developed sinusoidal obstruction syndrome/veno-occlusive disease. One pt had grade 1 CRS, and 2 pts had grade 1 tremor.
With a median follow-up of 13.4 months (range, 0.5-20.6 months), 6 pts (29%) have died (1 in the frontline cohort, 1 in the MRD cohort and 4 in the R/R cohort). 3 deaths were due to complications of alloSCT, 2 were due to sepsis (1 in the setting of refractory leukemia and 1 during MRD-negative CR), and 1 from unknown cause. Among 18 responding pts, only 1 pt relapsed; the pt with MRD-positive t(4;11) by FISH relapsed 4.5 months after alloSCT. The median OS for the R/R cohort was 5.8 months and was not reached for the frontline or MRD cohorts. The 1-year OS rate for the frontline + MRD cohort was 83%.
Conclusion: Dose-dense mini-hyper-CVD in combination with InO and Blina achieves rapid MRD-negative remissions in patients with B-cell ALL. All responding patients achieved flow MRD negativity after 1 cycle of therapy, with the majority also achieving NGS MRD negativity. This regimen is now being prospectively evaluated in an ongoing clinical trial in pts with R/R B-cell ALL and in older adults with newly diagnosed B-cell ALL.
Disclosures
Jain:Pharmacyclics: Consultancy, Honoraria, Other: Travel, Accommodations, Expenses, Research Funding; Mingsight: Research Funding; Newave: Research Funding; BMS: Consultancy, Honoraria, Other: Travel, Accommodations, Expenses, Research Funding; CareDX: Consultancy, Honoraria, Other: Travel, Accommodations, Expenses; AstraZeneca: Consultancy, Honoraria, Other: Travel, Accommodations, Expenses, Research Funding; Ipsen: Consultancy, Honoraria, Other: TRAVEL, ACCOMMODATIONS, EXPENSES; Janssen: Consultancy, Honoraria, Other: Travel, Accommodations, Expenses; Servier: Research Funding; Takeda: Research Funding; Pfizer: Research Funding; TransThera Sciences: Research Funding; Medisix: Research Funding; Novalgen: Research Funding; Adaptive Biotechnologies: Consultancy, Honoraria, Other: Travel, Accommodations, Expenses, Research Funding; Fate Therapeutics: Research Funding; Kite/Gilead: Consultancy, Honoraria, Other: Travel, Accommodations, Expenses, Research Funding; Dialectic Therapeutics: Research Funding; Loxo Oncology: Research Funding; Precision Biosciences: Consultancy, Honoraria, Other: Travel, Accommodations, Expenses, Research Funding; TG Therapeutics: Consultancy, Honoraria, Other: Travel, Accommodations, Expenses; MEI Pharma: Consultancy, Honoraria, Other: TRAVEL, ACCOMMODATIONS, EXPENSES; ADC Therapeutics: Research Funding; Genentech: Consultancy, Honoraria, Other: Travel, Accommodations, Expenses, Research Funding; AbbVie: Consultancy, Honoraria, Other: Travel, Accommodations, Expenses, Research Funding; Incyte: Research Funding; Aprea Therapeutics: Research Funding; Cellectis: Consultancy, Honoraria, Other: Travel, Accommodations, Expenses, Research Funding; Beigene: Consultancy, Honoraria, Other: Travel, Accommodations, Expenses. Ravandi:Abbvie: Consultancy, Honoraria, Research Funding; Celgene/BMS: Consultancy, Honoraria, Research Funding; Astellas: Consultancy, Honoraria, Research Funding; Astex/taiho: Membership on an entity's Board of Directors or advisory committees, Research Funding; Biomea fusion: Honoraria, Research Funding; Amgen: Honoraria, Research Funding; Xencor: Research Funding; Prelude: Research Funding; Syros: Consultancy, Honoraria, Research Funding. Konopleva:Abbvie, Allogene Therapeutics, Cellectis, Forty Seven, Gilead Sciences, Genentech, Sanofi, MEI Pharma, Rafael Pharmaceuticals, Daiichi Sankyo Pharmaceutical, AstraZeneca Co., Menarini, Precision BioSciences.: Research Funding; AbbVie, Forty Seven, Precision Biosciences, Gilead Sciences, Genentech, Janssen, Sanofi, MEI Pharma, Daiichi Sankyo Pharmaceutical, AstraZeneca Co., Menarini.: Consultancy; Reata Pharmaceuticals.: Current holder of stock options in a privately-held company, Patents & Royalties. Jabbour:Genentech: Consultancy, Honoraria, Research Funding; Pfizer: Consultancy, Honoraria, Research Funding; Takeda: Consultancy, Honoraria, Research Funding; Ascentage Pharma Group: Consultancy, Honoraria, Research Funding; Bristol-Myers Squibb: Consultancy, Honoraria, Research Funding; Abbvie: Consultancy, Honoraria, Research Funding; Adaptive Biotech: Consultancy, Honoraria, Research Funding; Amgen: Consultancy, Honoraria, Research Funding; Hikma Pharmaceuticals: Consultancy, Honoraria, Research Funding. Short:Novartis: Consultancy; AstraZeneca: Consultancy; Astellas: Research Funding; Stemline therapeutics: Research Funding; Takeda: Consultancy, Research Funding; Amgen: Honoraria; Pfizer: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal